File: chagasdisease.htm> <Medical Index> <General Index> Site Description Glossary <Navigate
to Home>
|
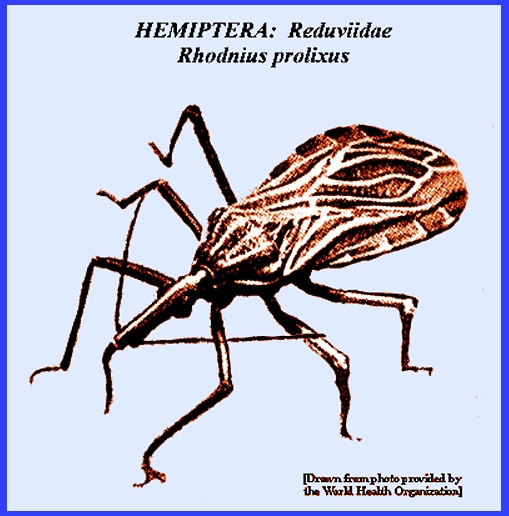
CHAGAS DISEASE (Contact) Please
CLICK on
image & underlined links for details: [See: Hemiptera
Key] LIFE CYCLE & BEHAVIOR In the
Hemimetabolous life cycle the eggs hatch after 10-15 days incubation to
produce small nymphs that resemble adults and which go through about five
stages of development. Like the
adults, the nymphs feed on blood, doing so mainly at night. They tend to seek out a host's head area for their blood meals. People are not normally aware that feeding
has occurred because there is little sensation. Detection of their presence is by observing cast molting skins
and streaks of fecal material in the houses.
The life cycle is quite long: about 3-10 months or sometimes even 1-2
years (Service 2008). All stages are
able to survive for several months without a blood meal. A large array of wild animals, including
squirrels mice, lizards and cattle, are attacked and may serve as reservoir
hosts. The vectors ingest the parasite's
trypomastigotes that reside in a host during a blood meal. The parasites then continue their
development within the insect's intestines.
There they further develop into epimastigotes and multiply to great numbers. Within 8 to 17 days these develop into
infective metacyclic trypomastigotes
in the lumen of the insect's posterior intestines. Vectors will regularly feed for 10-25 minutes or longer,
during which time many species of bugs excrete liquid or semi liquid feces
that may be contaminated with the metacyclic form of Trypanosoma cruzi that were derived from
an earlier blood meal. Infection in
humans occurs when bug excreta are scratched either into skin abrasions or
through the wound of the bug's bite, or when it might be rubbed into the eyes
or other mucous membranes.
Transmission results then only through the insect's feces and not
directly by its bite. Service
(2008) reported that there are some 70 species of Reduviidae that have been
found infected with T. cruzi,
but only about 12 species that live in close association with humans and feed
on them. Principal vector species are
Triatoma infestans
(southern South America), Pangastrongylus
megistus (southeastern Brazil), Rhodnius
prolixus (Honduras, Nicaragua, Colombia & Venezuela) and Triatoma dimidiata (Mexico
through northwestern South America).
The efficiency of a vector depends on how long it feeds on a human and
if it defecates during feeding.
However, Trypanosoma rangeli
that occurs from Mexico to Brazil and is transmitted by Rhodnius prolixus,
can infect humans directly by its bite. A further
discussion of the disease organism given by Service (2008) explained that Trypanosoma cruzi is really a parasite
of wild animals, such as opossums, armadillos and wild and urgan rats mice,
squirrels, monkeys, etc. that may serve as reservoir hosts. Simply eating the vectors or infected
animals can infect them. In some cases
humans can also aquire infection by eating infected meat or food that is contaminated
with infective bug excrement. The insect itself may also be an infection
reservoir, but in some areas humans are thought to be the main reservoir
hosts. Infection
rates in vector populations can frequently be very high. Service (2008) reported that it is common
to find infection rates of around 25 percent or higher. In California the Triatoma protracta
population can be 78 percent, but it rarely bites humans. Although vectors can account for more than
80 percent of transmission, blood transfusions account for 17 percent and
congenital transmission 2 percent. CONTROL Chagas
Disease is generally controlled by insecticide applications to the interior
surfaces of dwellings even though resistance to the insecticide develops
rapidly. Fumigation is effective but
must be done regularly. More
permanent but expensive control involves altering dwelling structures so as
to make them less attractive vector resting sites. Service (2008) noted that such alterations include plastering
walls to cover cracks and replacing thatched dwellings with those constructed
with bricks or concrete blocks, and having metal roofs. Because of the high rates of infection
among the human populations of northwestern South America, governments there
are launching massive efforts to inform and assist the public in vector
control. = = = = = = = = = = = =
= = = = = = = = Key References: <medvet.ref.htm> <Hexapoda> Barrett, T. V. 1991.
Advances in triatomine bug ecology in relation to Chagas disease. Advances in Disease Vector Research 8: 1843-76. Beard, C. R., C.
Cordon-Rosales & R. V. Durvasula.
2002. Bacterial symbionts and
their potential use in control of Chagas disease transmission. Ann. Rev. Ent.
47: 123-41. Brenner, R. R. &
A. M. Stoka. 1988. Chagas Disease Vectors I: Taxonomic,
Ecological & Epidemiological Aspects.
CRC Press, Boca Raton, FL. Bryan, R. T., F.
Balderrama, R. J. Tonn & J. C. P. Dias.
1994. Community participation
in vector control: lessons from
Chagas disease. Amer. J. Trop. Medicine &
Hyg. 50: 61-71. Carcavallo, R. U., I. G.
Galfndez-Giron, J. Jurberg & H. Lent.
1999. Atlas of Chagas Disease
Vectors in the Americas, Vol. 3, Rio de Janeiro: Oswaldo Cruz Fundacion. Kingman, S. 1991.
South America declares war on Chagas disease. New Scientist (19 Oct) pp. 16-17. Lent, H. & P.
Wygodzinsky. 1979. Revision of the Triatominae (Hemiptera,
Reduviidae), and their significance as vectors of Chagas disease. Bull.Amer. Mus. Nat. Hist. 163:
123-520. Matheson, R. 1950. Medical Entomology. Comstock Publ. Co, Inc. 610 p. Moncayo, A. & M. I.
Ortiz-Yanine. 2006. An update on Chagas disease (human
trypanosomiasis). A.. Trop. Med.
& Parasit. 100: 663-77. Schofield, C. J. &
J. P. Dujardin. 1997. Chagas disease vector control in Central
America. Parasitology Today 13: 141-44. Service, M. 2008.
Medical Entomology For Students.
Cambridge Univ. Press. 289 p Legner, E. F. 1995. Biological control of Diptera of medical and veterinary
importance. J. Vector Ecology 20(1):
59_120. Legner, E. F. 2000.
Biological control of aquatic Diptera. p. 847_870.
Contributions to a Manual of Palaearctic Diptera, Vol. 1, Science Herald, Budapest. 978 p. Yamagata, Y. & J. Nakagawa. 2006. Control of Chagas disease.
Adv. in Parasitology 61:
129-65. |