File: <scabies.htm> <Medical
Index> <General Index> Site Description Glossary <Navigate
to Home>
|
SCABIES (Contact) Please CLICK on
Image & underlined links for details: The rash is a
papular allergic eruption that is found on the body where the mites are not
present. First time mite infections
are followed 2-6 weeks later by the rash, while those how have had previous
infections will experience the rash within only 2-4 days (Service 2008). Itch and scratching can follow an
infection, which can then lead to serious secondary bacterial infections. A
very serious form of scabies known as "Crusted
Scabies" or "Norwegian
Scabies" can involve thousands of mites. LIFE CYCLE The mite
females excavate below the skin's surface where it is thin as around wrists,
fingers, feet, etc. However, most are
found on the hands and wrists and sometimes they also infest the head region
of their hosts. Once under the skin
females create winding tunnels and feed on liquids produced by the dermal
cells. About 1-3 eggs are laid daily
in the tunnels, which then require about four days to hatch with small larvae
that have only six legs. The larvae
migrate to the skin's surface where most perish, but the survivors seek out a
hair follicle where they moult and develop into a "protonymph) with
eight legs. A "tritonymph"
is produced after about 3-4 days.
Service (2008) noted that female nymphs are much larger than male
nymphs. About 3 days later the
tritonymph moults to produce either a male or female adult. Mated females then increase their size and
begin their penetration into skin.
Males, on the other hand, are much smaller and wander about the skin
surface and construct short dens for refuge.
The total life cycle usually requires less than two weeks, and females
may live up to six weeks on their hosts, but perish in a few days without
hosts. MEDICAL IMPORTANCE Skin diseases, known as Scabies, Acariasis, Sarcoptic
Itch, etc., are produced in humans and animals. Some of the Sarcoptes spp.
actually inhabit tunnels underneath the skin. These mites may pass their entire lives on their hosts. Infestations among hosts are acquired by
contact. It has been estimated that
over 300 million cases of Scabies
occur annually worldwide. One family,
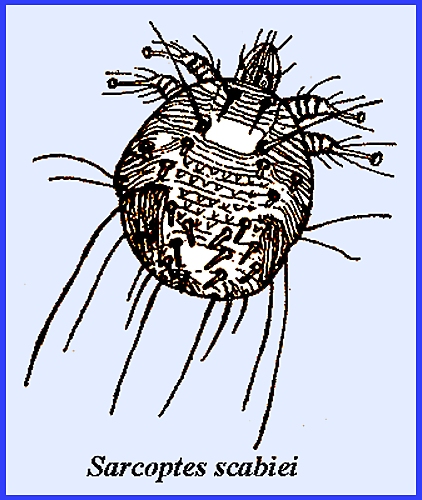
Sarcoptidae, and genus, Sarcoptes, is of
principal importance for humans. Sarcoptes scabiei is known as the "Human Itch Mite," of "Norwegian Itch" as it is sometimes
called. Females that are larger than
males have the dorsal part of the body marked with distinctive parallel
lines. The mites locate in the upper
layers of epidermis especially around the groin and more sequestered areas. Mature females that bore directly into
skin where they remain concealed for a while construct egg tunnels. Enlarging the excavation and laying eggs
follow this. Eggs hatch in 3-4 days
and the larvae leave the tunnel for the skin surface where they enter hair
follicles. Molting occurs in 2-3 days
followed by two nymphal stages.
Nymphs construct narrow tunnels where mating occurs. The life cycle varies from 8-15 days at
room temperature. Adult longevity is
3-5 weeks. A person may
acquire 50 or more mites at any given time, and any infections that develop
are not obvious for several weeks.
Following an attack there are at first few symptoms. Gradually as one becomes sensitized an
intense itching ensues, which is especially intense at night. Infections are more likely the more one
scratches the infested areas. Acquisition
of mites is through close contact with infested persons or their
clothing. Avoidance of infested areas
is preferred, but if infected one should seek medical attention from a physician,
for current products available for treatment. There are
also species (eg., Psoroptes communis and Notoedres cati itch mites
attacking animals that do not tunnel bur rather possess suckers for exterior
attachment to the skin. Humans only
become affected from close contact with infested animals, such as cats and
rats. CONTROL Scabies may
be controlled by the application of medicated skin lotions, sulphur ointments
and other compounds (Buffet & Dupin 2003, Service 2008). Because scabies is contagious it may be
necessary to deploy control procedures to entire families or even
communities. Relief from the rash
only gradually disappears after treatments.
The attention of a medical physician is advised for this group of
mites, as medicinal treatment is usually required. Prevention involves the usual precautions of cleanliness and
limiting contact with infected surfaces, animals and people. However, Service (2008) recommended that
during epidemics clothing and bedding should be dry cleaned or washed in
50-deg. Centigrade water. = = = = = = = = = = = =
= = = = = = = = Key References: <medvet.ref.htm> <Hexapoda> Arlian, L. C. 1989.
Biology, host relations and epidemiology of Sarcoptes scabiei. Ann. Rev. Ent. 34: 139-61. Arlian, L. G. &
M. S. Morgan. 2000. Serum antibody to Sarcoptes
scabiei and house dust mite prior
to and during infestation with S.
scabiei. Vet. Parasitol. 90:315326. Arlian, L. G.,
Morgan MS, Neal J.S. 2003. Modulation
of cytokine expression in human keratinocytes and fibroblasts by extracts of
scabies mites. Am J Trop. Med Hyg. 69: 652656 Arlian, L. G., M. S.
Morgan, & J. S. Neal. 2004. Extracts of scabies mites (Sarcoptidae: Sarcoptes
scabiei) modulate cytokine
expression by human peripheral blood mononuclear
cells and dendritic cells. J Med Entomol. 41: 6973. Arlian, L. G., M. S.
Morgan, C. M. Rapp & D. L. Vyszenski-Moher. 1996. The development of protective immunity in
canine scabies. Vet. Parasitol. 62: 133142. Arlian, L. G., C. M. Rapp, B. L. Stemmer, M. S. Morgan
& P. F. Moore. 1977. Characterization
of lymphocyte subtypes in scabietic skin lesions of naοve and sensitized dogs. Vet. Parastitol. 68: 347358. Arlian, L. G., C. M.
Rapp, D. L. Vyszenski-Moher & M. S. Morgan. 1994. Sarcoptes
scabiei: Histopathological changes
associated with
acquisition and expression of host immunity to scabies. Exp. Parasitol. 78: 5163. Buffet, M. & N.
Dupin. 2003. Current treatments for scabies. Fund. & Clinical Pharmacology 17: 217-25 Cox, N. H. 2000.
Permethrin treatment in scabies infestation: importance of the correct formulation. BMJ 300:
37-38. Daisley, H., W. Charles & M. Suite. 1993.
Crusted (Norwegian) scabies as a pre-diagnostic indicator for HTLV-1
infection. Trans. Roy. Soc. Trop Med & Hyg. 87: 295. Kemp,
D. J, S. F. Walton, P. Harumal, & B. J. Currie . 2002.
The scourge of scabies. Biologist. 49: 1924. Matheson, R. 1950. Medical Entomology. Comstock Publ. Co, Inc. 610 p. Marliere, V., S. Roul, C. Labreze & A.
Taieb. 1999. Crusted (Norwegian) scabies induced by use
of topical corticosteroides and treated successfully with ivermectin. J. Pediatrics 135: 122-124. Meinking, T. L. , C. N. Burkhart & C. G.
Burkhart. 1999. Ectoparasitic diseases in
dermatology: reassessment of scabies
and pediculosis. Adv. in Dermatology 15:
77-108. Meinking, T. L. & G.
W. Elgart. 2000. Scabies therapy for the millenium. Pediatric Dermatology 17: 154-56. Mullen, G. & B. M. O'Connor. 2002.
Mites (Acari). In: Medical
& Veterinary Ent., ed. G. Mullen & L. Durden, Amsterdam Acad. Press,
pp 449- 516. Orkin, M. & H. T.
Maibach (eds.). 1985. Cutaneous Infestations & Insect
Bites. Marcel Dekker, New York. Service, M. 2008.
Medical Entomology For Students.
Cambridge Univ. Press. 289 p Turner, S., S. Lines, Y. Chen, I. Hussey & R.
Aguis. 2005. Work-related infectious
disease reported to the Occupational Disease Intelligence Network & the Health & Occupation Reporting Network in the UK
(2000-2003). Occupational Medicine
(London). 55: 275-281. Walker, G. J. A. & P. W. Johnstone. 2000. Interventions for
treating scabies. Archives of
Dermatology 136: 387-89. |